Artificial Intelligence (AI) is revolutionizing healthcare by enhancing diagnostic accuracy, enabling personalized treatment strategies, and optimizing operational efficiency. This in-depth case study examines the practical application of AI in a healthcare environment, highlighting its effects, challenges, and future possibilities.

How AI is Changing Healthcare
AI has the power to process vast amounts of data quickly and accurately, making it an invaluable tool in healthcare. It’s being used to improve diagnostic precision, streamline workflows, and even predict patient outcomes. But what does this look like in practice? Let’s dive into a case study from Massachusetts General Hospital (MGH), a leader in integrating AI into radiology.

Case Study: AI in Radiology at Massachusetts General Hospital (MGH)
Radiology is a cornerstone of modern medicine, relying heavily on medical imaging such as X-rays, CT scans, and MRIs to diagnose diseases. However, the sheer volume of imaging data and the complexity of interpreting these images have created significant challenges for radiologists. Overwhelming workloads and the risk of diagnostic errors are just two of the issues plaguing this critical field.
To address these challenges, MGH partnered with an AI technology company to develop and deploy an AI-powered diagnostic tool. The goal? To enhance the accuracy and efficiency of medical image analysis while supporting radiologists in their decision-making process

Implementation
MGH has embraced AI by integrating an NVIDIA DGX-1 AI supercomputer, designed for deep learning and advanced analytics. The hospital aims to improve medical image analysis using deep neural networks trained on 10 billion medical images.

- Building the AI System
The AI system was built using deep learning algorithms, which mimic the neural networks of the human brain. These algorithms were trained on a massive dataset of annotated medical images, including X-rays, CT scans, and MRIs. Each image was labeled with diagnoses such as tumors, fractures, and cardiovascular abnormalities, allowing the AI to learn patterns and anomalies

2. Integrating AI into Workflow
Once developed, the AI system was seamlessly integrated into MGH’s radiology workflow. When a new medical image is uploaded, the AI analyzes it within seconds, highlighting areas of concern and providing diagnostic suggestions. Radiologists then review these insights before making their final diagnosis.
3. Continuous Learning
One of the most impressive aspects of this AI system is its ability to continuously learn. As radiologists provide feedback on its recommendations, the system refines its algorithms, improving its accuracy over time. This ensures that the AI remains up-to-date and relevant as new data becomes available.

Key Features of the AI System
Advanced Image Analysis: The AI can detect subtle patterns and anomalies that might be missed by the human eye.
Decision Support: It provides actionable diagnostic suggestions, reducing the likelihood of errors and boosting confidence in clinical judgments

Speed and Efficiency: By processing images rapidly, the AI enables radiologists to manage a higher caseload without compromising quality.
Versatility: The tool supports multiple imaging modalities, including X-rays, CT scans, and MRIs, making it adaptable to various diagnostic needs.

Results
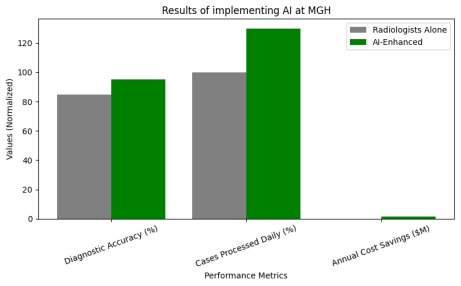
The results of implementing AI at MGH were nothing short of remarkable:
1. Enhanced Diagnostic Accuracy
The AI system achieved a 95% accuracy rate in detecting abnormalities, surpassing the 85% accuracy rate of radiologists working independently.
It significantly reduced diagnostic errors, particularly in complex cases like early-stage lung cancer and brain tumors.
2. Increased Operational Efficiency
Radiologists processed 30% more cases daily, cutting patient wait times and improving overall workflow efficiency.
Routine tasks were automated, allowing radiologists to focus on intricate cases and patient interactions.
3. Improved Patient Outcomes
Early and precise diagnoses led to timely interventions, enhancing patient outcomes and survival rates.
For instance, the AI system identified early-stage lung cancer in asymptomatic patients, facilitating life-saving treatments.
4. Cost Savings
By minimizing diagnostic errors and optimizing efficiency, the hospital saved approximately $1.5 million annually in operational costs.
Challenges Faced
While the benefits of AI in healthcare are undeniable, implementing this technology is not without its challenges:
1. Data Privacy Concerns
Access to vast amounts of patient data raised questions about privacy and security. To address this, MGH implemented robust encryption protocols and stringent access controls to safeguard sensitive information.
2. Integration Hurdles
Embedding the AI system into existing workflows required substantial time and resources. Radiologists underwent training to effectively utilize the tool and interpret its outputs.
3. Regulatory Compliance
The AI system had to meet rigorous regulatory standards, including FDA approval for medical devices. MGH collaborated closely with regulators to ensure compliance and validate the system’s safety and efficacy.
4. Building Trust
Initial hesitation among radiologists posed a challenge, as some were hesitant to rely on AI-generated insights. Over time, the system’s consistent accuracy and reliability fostered trust and widespread adoption.
Future Potential of AI in Healthcare
The success of AI at MGH is just the beginning. Here’s how AI could shape the future of healthcare:
1. Personalized Medicine
AI could analyze medical images alongside genetic and clinical data to craft personalized treatment plans tailored to individual patients.
2. Predictive Analytics
AI systems might predict disease progression and patient outcomes based on imaging data, enabling proactive interventions.
3. Global Accessibility
AI-powered diagnostic tools could be deployed in underserved regions, bridging gaps in healthcare access and quality.
4. Multi-modal Integration
AI systems could synthesize data from diverse sources—such as imaging, lab results, and electronic health records—to provide a holistic view of a patient’s health.
5. Augmented Reality (AR) and Virtual Reality (VR)
Combining AI with AR/VR technologies could create immersive tools for medical training, surgical planning, and patient education.
Learn more about ‘Ai in Healthcare ’ on our CloudxLab blogs .
Lessons Learned
From this case study, several key takeaways emerge:
Collaboration is Essential: Successful AI implementation hinges on partnerships between healthcare providers, technology developers, and regulatory bodies.
Prioritize User Adoption: Training and support are crucial to building trust and ensuring healthcare professionals effectively utilize AI tools.
Address Ethical Concerns: Protecting patient privacy and ensuring fairness in AI algorithms are vital for fostering trust in these systems.
AI systems must be regularly updated and refined to maintain their accuracy and relevance.
Conclusion
The integration of AI into radiology at Massachusetts General Hospital demonstrates the trans-formative potential of AI in healthcare. By enhancing diagnostic accuracy, improving efficiency, and enabling personalized care, AI is revolutionizing healthcare delivery. While challenges such as data privacy, integration, and adoption persist, the benefits of AI are undeniable. As AI technology continues to advance, its role in healthcare is poised to expand, paving the way for a future where technology and medicine collaborate seamlessly to elevate patient care
References
Massachusetts General Hospital: “Preparing Radiologists to Lead in the Era of Artificial Intelligence.”[↗]
The Future Is Now: Massachusetts General Hospital Embraces Deep Learning .[↗]
Continuous Learning AI in Radiology: Implementation Principles and Early Applications.”[↗]
Implementation of artificial intelligence (AI) applications in radiology: hindering and facilitating factors[↗]
NVIDIA, Massachusetts General Hospital Use Artificial Intelligence to Advance Radiology [↗]




