Cancer is one of the leading causes of death worldwide, with millions of new cases diagnosed every year. The key to improving survival rates is early detection, as cancers caught in their initial stages are significantly more treatable. Traditional diagnostic methods, such as biopsies, CT scans, MRIs, and mammograms, have limitations in accuracy, speed, and accessibility.
This is where Artificial Intelligence (AI), Machine Learning (ML), and Deep Learning (DL) are making a creative impact. AI-driven cancer detection systems are improving accuracy, reducing diagnostic time, and making cancer screening more accessible to populations worldwide. This blog explores how AI is transforming early cancer detection, its history, current advancements, and future potential.
A Brief History of Cancer Detection
Before modern medical imaging, cancer detection relied heavily on physical symptoms and biopsy procedures. By the late 19th and early 20th centuries, X-rays and microscopy became essential tools for identifying abnormal growths. However, misdiagnosis rates were high due to human limitations in analyzing medical images.
Early Efforts (1950s-2000s)
- In the 1950s and 1960s, researchers explored rule-based systems for medical diagnosis, though computational power was limited.
- The 1990s saw the first computer-aided detection (CAD) systems for breast cancer, primarily analyzing mammograms for microcalcifications.
- By the early 2000s, digital imaging became more widespread, enabling researchers to train models on medical scans.
Advancements in AI (2010s – Present)
- The rise of Deep Learning (2010s) enabled AI models to process vast amounts of medical imaging data, outperforming traditional CAD methods.
- Google’s DeepMind and other AI research labs developed AI models capable of detecting cancerous lesions more accurately than human radiologists.
| Feature | Traditional Methods | AI-Powered Detection |
| Accuracy | 75-85% (Varies by Cancer Types) | 90-98% (Higher accuracy in early detection) |
| Speed | Takes days or weeks for results | Immediate or within minutes |
| Human Error | Prone to misdiagnosis & interpretation errors | Reduce false positives & false negatives |
| Scalability | Requires highly trained specialists | AI can analyze thousands of scans instantly |
| Cost | Expensive, especially in low-income areas | Reduces overall costs by early intervention |
AI vs. Traditional Cancer Detection Methods (Comparison Chart)
Present Scenario: AI in Cancer Detection Today
AI is now widely used in various aspects of cancer screening, diagnosis, and treatment planning.
AI-powered Cancer Screening Tools
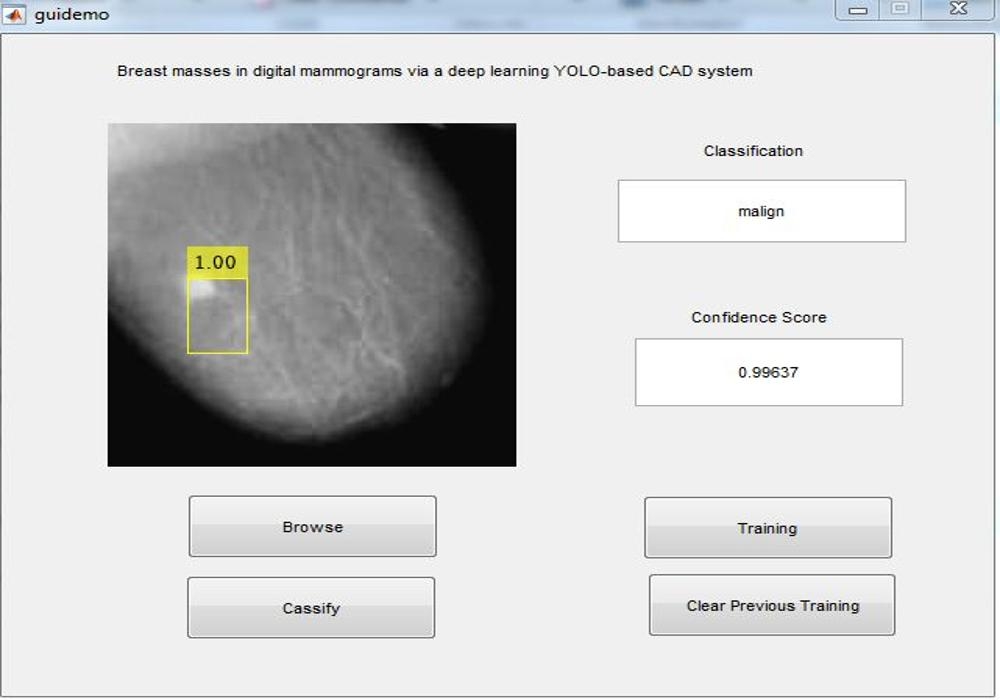
1. Breast Cancer Detection
- AI models analyze mammograms to detect tumors at an early stage.
- Example: AI models reduced false positives and false negatives in breast cancer screenings. Link
2. Lung Cancer Detection
- AI-powered CT scan analysis helps detect lung nodules before they develop into advanced cancer.
- Example: Deep Learning models trained on low-dose CT scans have improved early detection rates. Link
3. Skin Cancer Detection
- AI algorithms analyze skin lesions and classify them as benign or malignant based on dermatoscopic images.
- Example: Stanford University’s AI model achieved dermatologist-level accuracy in melanoma detection. Link
4. Cervical Cancer Screening
- AI analyzes Pap smears and HPV test results to identify precancerous lesions.
- Example: AI-assisted digital colposcopy in low-resource areas is improving early detection rates. Link
How AI Detects Cancer: The Technology Behind It
AI-driven cancer detection is built upon advanced machine learning (ML) and deep learning (DL) techniques that analyze medical images, genetic data, and pathology slides. These AI models aim to mimic human radiologists and pathologists, identifying cancerous patterns with higher accuracy and efficiency. Here’s a step-by-step breakdown of how the technology works:
1. Data Collection & Preprocessing
AI models rely on large-scale medical datasets to learn and improve accuracy. The quality of the data is crucial in developing reliable AI-based cancer detection systems.
Types of Data Used
a) Medical Imaging Data:
- X-rays, CT scans, MRIs, PET scans -> Detect Lung, brain, and breast cancer.
- Mammograms & Ultrasounds -> Used for breast cancer screening.
- Dermatoscopic Images -> Analyzes skin lesions for melanoma detection.
- Histopathology Slides -> Microscopic examination of tissue samples to detect abnormal cell structures.
b) Genetic & Molecular Data:
- DNA sequencing -> AI can analyze mutations in genes like BRCA1/BRCA2 (linked to breast cancer).
- Liquid Biopsies -> AI can detect circulating tumor DNA (ctDNA) in blood tests.
c) Clinical & Patient Data:
- Electronic Health Records (EHRs) -> AI can analyze patient history to identify risk factors.
Preprocessing Techniques
Before AI models can learn from the data, preprocessing is required to enhance accuracy:
- Normalization: Standardizing image brightness and contrast.
- Noise Reduction: Removing irrelevant details from scans (e.g., blurring artifacts in X-rays).
- Data Augmentation: Rotating, flipping, and scaling images to help AI learn from varied perspectives.
- Segmentation: Separating cancerous areas from healthy tissues using AI-driven image segmentation techniques.
2. Machine Learning & Deep Learning Models
AI uses various ML and DL models to detect cancer with high precision.
a. Convolutional Neural Networks (CNNs) – For Image Recognition
CNNs are the backbone of cancer detection in medical imaging. They analyze pixel-level patterns in scans to distinguish between normal and cancerous tissues.
How it Works:
- Feature Extraction: The CNN learns hierarchical features from an image (edges, shapes, textures).
- Convolutional Layers: The model applies multiple filters to detect abnormalities.
- Pooling Layers: Reduces the spatial dimensions while preserving important features.
- Fully Connected Layers: Classifies the image as “Cancerous” or “Non-Cancerous.”
Example:
Google DeepMind’s AI model outperformed human radiologists in breast cancer detection by analyzing mammograms using CNNs. Link
b. Recurrent Neural Networks (RNNs) – For Time-Series Analysis
Use Case:
Predicting cancer progression over time (e.g., tumor growth rate from past scans).
Example:
AI models analyze multiple MRI scans over months to assess whether a tumor is growing aggressively.
c. Transformer Models – For Analyzing Textual Data (Pathology Reports)
Use Case:
AI reads pathology reports and medical literature to assist doctors in making better diagnoses.
Example
IBM Watson Health uses transformer-based NLP models to extract insights from oncologists’ notes and research papers. Link
3. AI Training Process
For AI models to become effective at detecting cancer, they must undergo rigorous training using large labeled datasets.
a. Supervised Learning – Training AI with Labeled Data
Supervised learning is the most common AI approach used in cancer detection. In this method, AI models are trained on large datasets of labeled medical images, where each image is tagged as cancerous or non-cancerous by expert radiologists. The model learns to recognize patterns and improve its accuracy over time.
How Supervised Learning Works in Cancer Detection:
- Large Labeled Datasets: AI is trained on thousands of X-rays, CT scans, MRIs, and histopathology slides that have been labeled by oncologists.
- Pattern Recognition: The AI identifies common visual features of tumors, such as irregular shape, density, and contrast differences.
- Error Correction: The model is fine-tuned by comparing its predictions to the correct labels, gradually reducing false positives (incorrectly flagging healthy tissue) and false negatives (missing cancerous regions).
- Feature Engineering: AI extracts key characteristics like tumor size, shape, texture, and contrast to improve classification.
- Confidence Scoring: AI provides a probability score for each prediction, helping radiologists assess uncertainty.
Example Use Case:
- DeepMind’s AI for Breast Cancer Detection: A supervised deep learning model was trained on over 90,000 mammograms, learning to identify cancerous growths with higher accuracy than human radiologists in some cases. Link
b. Reinforcement Learning – Continuous Improvement
Reinforcement Learning (RL) allows AI models to continuously improve by learning from feedback. Instead of just making predictions, RL models receive rewards or penalties based on the accuracy of their outputs, helping them refine their decision-making over time.
How Reinforcement Learning Enhances Cancer Detection:
- Human-in-the-Loop Learning: AI suggestions are reviewed by radiologists. If a mistake is found, the system updates its learning process.
- Adaptive Learning: Over time, AI models learn to distinguish subtle cancerous patterns, improving accuracy in edge cases.
- Confidence Calibration: AI assigns confidence scores to its predictions and learns to be more certain when patterns are clear.
- Active Learning: AI prioritizes difficult cases where it has low confidence and seeks human validation to enhance its training data.
Example:
- If the AI makes an incorrect prediction, doctors correct it, and the model adjusts its parameters accordingly.
c. Unsupervised Learning – Detecting Anomalies Without Labels
Unlike supervised learning, where AI models are trained on labeled datasets (cancerous vs. non-cancerous images), unsupervised learning detects patterns and anomalies without predefined labels. This is particularly useful in cancer detection for identifying rare, previously unknown tumor types.
How Unsupervised Learning Helps in Cancer Detection:
- Clustering Techniques: AI groups similar medical images together, helping radiologists discover new cancer subtypes.
- Anomaly Detection: AI detects outliers that may indicate rare or aggressive cancer forms not covered in traditional datasets.
- Feature Extraction: AI identifies unique characteristics of tumors that human experts might overlook.
- Reducing Labeling Effort: Medical datasets require extensive labeling by experts. Unsupervised AI can analyze vast datasets without manual labeling and find unknown correlations.
Example Use Case:
- AI in Brain Tumor Detection: An unsupervised model analyzes thousands of MRI scans and discovers a new subcategory of brain tumors based on subtle textural differences that were previously unnoticed by radiologists.
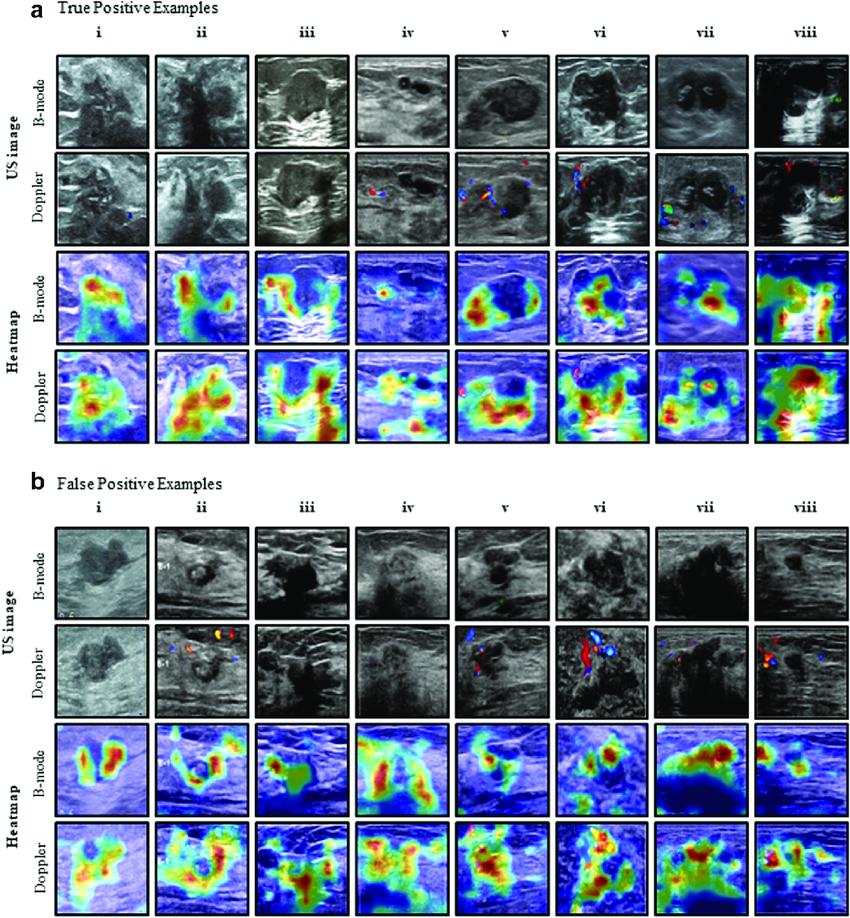
4. Explainability & AI Interpretability
One major challenge in AI adoption is its “black box” nature – meaning doctors may not always understand how AI reaches a decision. To solve this, researchers are developing Explainable AI techniques:
a. Heatmaps & Attention Maps
- AI generates saliency maps to highlight suspicious areas in an image.
- Example: Grad-CAM (Gradient-weighted Class Activation Mapping) shows doctors where the AI is “looking” in a mammogram. Link
b. Confidence Scores
- AI provides a probability score for cancer likelihood.
- Example: A model might say:
- “90% chance of lung cancer” -> High confidence, requires immediate attention.
- “40% chance of tumor” -> Uncertain, needs further tests.
c. Human-AI Collaboration
- AI does not replace doctors; it serves as a second opinion to assist radiologists.
- Example: AI flags high-risk cases for review, but a radiologist makes the final decision.
Challenges in AI Cancer Detection Today
While AI has shown immense promise in early cancer detection, several challenges must be addressed before it can be fully integrated into clinical practice. Below are the key hurdles:
1. Data-Related Challenges
a. Data Bias and Diversity Issues
- AI models are trained on medical imaging datasets, but many of these datasets lack diversity.
- If the AI is trained mostly on data from Western populations, it may not generalize well to patients from other ethnic or demographic backgrounds.
- Example: Studies have shown that some AI models perform worse on Black and Asian Patients because they were trained on predominantly Caucasian datasets.
Potential Solution:
- Collect more diverse datasets with images from various ethnicities, age groups, and geographic regions.
- Use data augmentation techniques to artificially increase dataset diversity.
b. Data Privacy and Security
- Medical imaging and patient records are highly sensitive data that require strict privacy regulations.
- AI training needs large datasets, but data sharing is restricted by laws like HIPAA (USA), GDPR (Europe), and similar regulations in other countries.
- Hospitals may be reluctant to share data due to liability and cybersecurity concerns.
Potential Solution:
- Use federated learning, where AI models are trained across multiple hospitals without transferring patient data.
- Implement strong encryption methods to protect patient information.
2. AI Model Performance & Reliability
a. Maximize recall instead of balancing it with precision
- In cancer detection, recall (the ability to correctly identify all cancerous cases) is more critical than precision (the percentage of identified cancer cases that are actually cancer).
- However, if precision is prioritized over recall, cancerous cases may be missed, which can be fatal.
Potential Solution:
- A high recall, low precision model detects nearly all cancerous cases.
- Setting a lower decision threshold to increase recall ensures that even subtle signs of cancer are flagged for further review.
- Instead of fully automating cancer detection, AI should assist radiologists by highlighting suspicious areas, which can then be verified manually.
- AI should continuously learn from false positives and false negatives by incorporating new cases into training, improving accuracy over time.
b. Overfitting and Lack of Generalizability
- Some AI models perform exceptionally well on specific datasets but fail when tested on real-world hospital data.
- This happens when models are overfitted – they learn patterns specific to the training data but don’t generalize to new cases.
Potential Solution:
- Train AI models on large, multi-institutional datasets rather than a single source.
- Use transfer learning, where an AI model pre-trained on one dataset is fine-tuned on new data.
3. Regulatory and Ethical Challenges
a. Regulatory Approval and Legal Compliance
- AI-based cancer detection tools must pass strict FDA (USA), EMA (Europe), and WHO regulations before deployment.
- Clinical validation trials take years, delaying AI adoption.
- If an AI tool makes a diagnostic mistake, who is legally responsible – the AI company, the hospital, or the doctor?
Potential Solution:
- Implement AI Explainability so regulators can understand how AI reaches decisions.
- Clearly define legal responsibility in case of AI-related errors.
b. Ethical Concerns in AI Decision-Making
- If AI recommends an aggressive cancer treatment, should doctors blindly follow it?
- Patients may lose trust in AI-driven diagnosis if they don’t understand how the AI reaches its conclusion.
Potential Solution:
- Use Explainable AI to provide visual or text-based explanations for each AI decision.
- Allow patients to request a human second opinion before undergoing major treatments.
4. Integration into Clinical Workflows
a. AI Adoption Resistance Among Doctors
- Many radiologists and oncologists fear that AI may replace their jobs, leading to resistance to adoption.
- Some doctors find AI hard to interpret, making them hesitant to trust its recommendations.
Potential Solution:
- Position AI as a decision-support tool, not a replacement for doctors.
- Provide training programs for medical professionals to learn how to use AI effectively.
b. Lack of Standardized AI Implementation in Hospitals
- Different hospitals use different imaging machines, storage systems, and electronic health records (EHRs), making it difficult to integrate AI models.
- AI software might not be compatible with legacy hospital infrastructure.
Potential Solution:
- Develop interoperable AI systems that can work with various hospital setups.
- Encourage government policies that push for standardized AI integration in healthcare.
5. Cost and Accessibility Issues
a. High cost of AI Implementation
- Developing, training, and deploying AI cancer detection models is expensive.
- Many hospitals, especially in developing countries, cannot afford AI-powered diagnostics tools.
Potential Solution:
- Create low-cost, cloud-based AI tools that hospitals can use without expensive infrastructure.
- Encourage public-private partnerships to fund AI-driven cancer detection programs in low-income regions.
b. Unequal Access to AI Cancer Screening
- AI-powered cancer screening is often only available in large, urban hospitals, leaving rural populations underserved.
- Patients in low-income countries may not have access to AI-driven diagnostics.
Potential Solution:
- Deploy mobile AI screening units in remote areas.
- Develop AI-assisted smartphone apps for basic cancer risk assessment.
Future of AI in Cancer Detection
As AI continues to evolve, its role in cancer detection is set to expand significantly. Future advancements will focus on precision, accessibility, real-time monitoring, and multi-modal analysis to enhance early detection rates and reduce mortality. Below are some key areas shaping the future of AI-driven cancer detection.
1. AI and Multi-Omics Data Integration
Cancer detection is no longer limited to imaging; future AI models will integrate various biological data sources, including:
- Genomics: AI will analyze a patient’s DNA to identify cancer-causing mutations (e.g., BRCA1/BRCA2 mutations in breast cancer).
- Proteomics: AI will study proteins expressed in cancerous tissues to detect specific biomarkers.
- Metabolomics: AI will examine metabolic changes in the body that signal early cancer development.
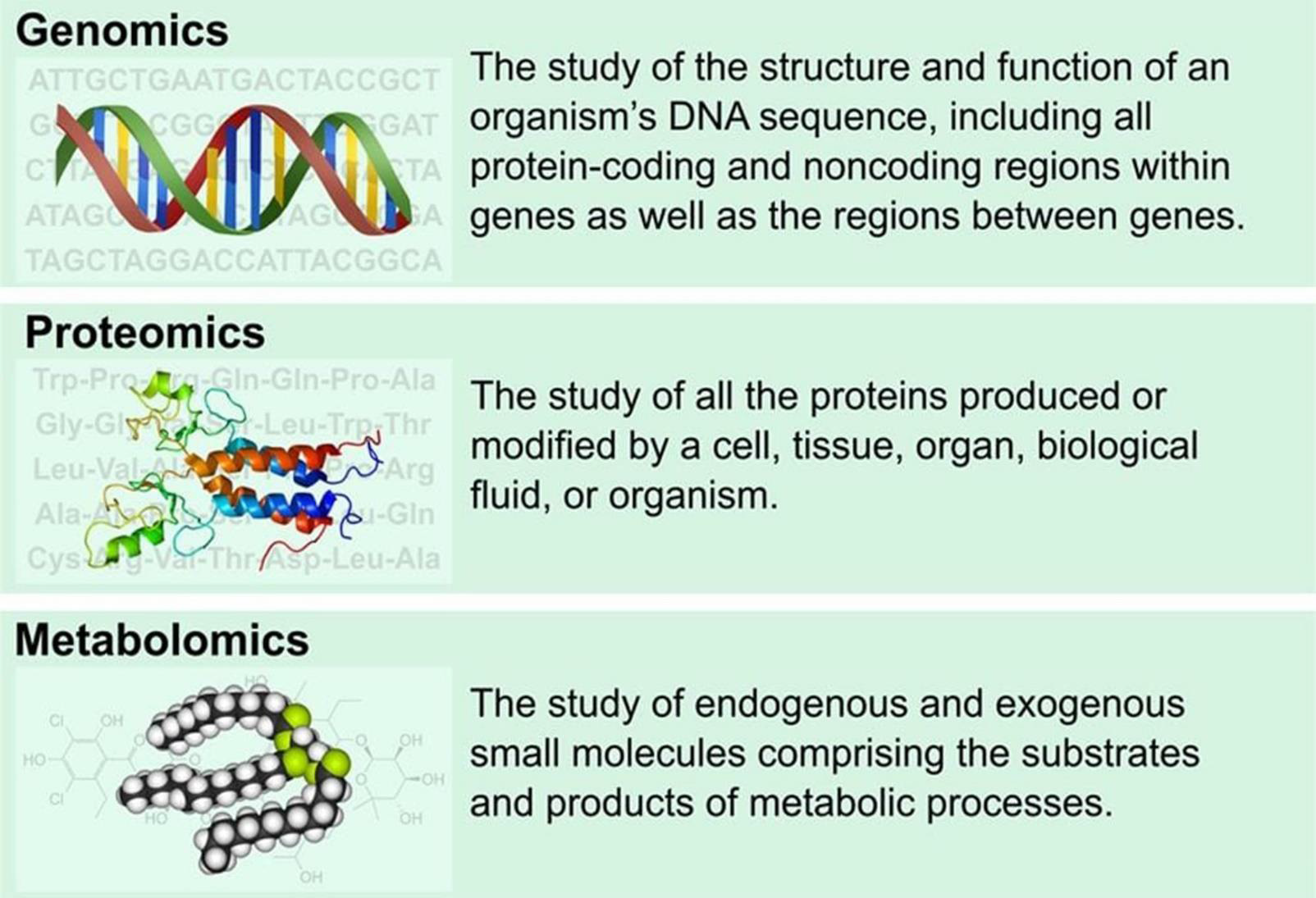
Real-World Implementation:
Researchers are developing AI-powered multi-omics platforms that analyze genetic and metabolic data to predict cancer risk years before symptoms appear. Link
2. Real-time AI in Wearable Devices and Liquid Biopsies
Wearable Technology is emerging as a game-changer in cancer detection. AI-powered biosensors in smartwatches and fitness trackers can analyze heart rate, skin temperature, oxygen levels, and molecular biomarkers to detect early cancer warning signs.
Additionally, liquid biopsies (non-invasive blood tests) will use AI to identify cancerous cells circulating in the bloodstream before tumors form.
Real-World Implementation:
- Stanford University has developed an AI-powered liquid biopsy that detects lung and pancreatic cancer with 92% accuracy before traditional imaging methods. Link
- Apple and Google are working on integrating AI-powered early cancer detection algorithms into wearable devices. Link
| Feature | Smartwatches (Apple, Fitbit) | AI-Powered Biosensors | AI-Driven Liquid Biopsies |
| Detection Types | Heart Rate, Skin Temperature | Blood Oxygen, Sweat analysis | Tumor DNA in blood |
| Cancer Types | Skin Cancer, General Wellness | Lung, Breast, Pancreatic | All Major Cancers |
| Availability | Commercially available | In Research & Testing | Limited clinical use |
AI & Wearable Devices for Cancer Detection (Comparison Chart)
3. AI-Enabled Robotic Biopsy & Surgery
AI-powered robotic systems are enhancing the accuracy, precision, and safety of cancer biopsies and surgeries.
- AI-guided robotic biopsies improve the accuracy of tissue sample collection, reducing the need for repeat procedures.
- AI-assisted robotic surgery enables more precise removal of cancerous tissue while preserving healthy surrounding tissue.
Real-World Implementation:
- The Da Vinci Surgical System, equipped with AI-assisted tools, is being used in minimally invasive cancer surgeries to enhance precision. Link
- AI-powered biopsy robots are being tested to automatically locate and extract cancerous tissue in prostate and breast cancer patients.
4. AI in Global Cancer Screening Programs
One of the biggest challenges in cancer detection is limited access to screening tools in developing countries. AI is set to democratize cancer detection by making screening cheaper, faster, and more accessible.
- AI-powered mobile screening units will bring early cancer detection tools to remote areas.
- Cloud-based AI platforms will allow radiologists in low-resource hospitals to upload scans and receive AI-driven diagnoses in real time.
- AI will reduce the burden on understaffed healthcare systems by automating initial cancer screenings.
Real-World Implementation:
- Google Health’s AI model is already being tested in Thailand and India for low-cost, AI-driven breast cancer screening in rural hospitals. Link
- Microsoft’s Project InnerEye is using AI to provide radiotherapy treatment planning for hospitals in low-income countries. Link
5. AI for Personalized Cancer Prediction & Treatment Planning
In the future, AI will not just detect cancer but also predict an individual’s risk based on lifestyle, genetics, and environmental factors.
- AI-driven predictive models will assess how likely a person is to develop cancer in their lifetime, allowing for proactive lifestyle changes.
- AI will generate personalized treatment plans by analyzing tumor characteristics, patient history, and genetic factors.
- AI-powered virtual oncologists will assist doctors by suggesting the best treatment options based on real-time data analysis.
Real-World Implementation:
- IBM Watson Oncology is already helping doctors in some hospitals by suggesting personalized cancer treatment plans based on big data analysis. Link
- Researchers at John Hopkins University are developing Artificial Tumors to help AI detect early-stage cancer. Link
6. AI-Driven Immunotherapy Advancements
Immunotherapy is one of the most promising cancer treatments, but only 20-40% of patients respond to it. AI will play a key role in:
- Predicting which patients will respond to immunotherapy.
- Identifying new immunotherapy drug targets by analyzing immune system interactions with cancer cells.
Real-World Implementations:
- DeepMind’s AlphaFold AI is helping researchers understand protein structures related to cancer and immune response, leading to potential new immunotherapy drugs. Link
- Memorial Sloan Kettering Cancer Center is using AI models to predict patient response to immunotherapy, increasing success rates. Link
7. The Role of Federated Learning in AI Cancer Detection
A major challenge in AI healthcare is data privacy – hospitals cannot easily share patient data due to strict regulations. Federated learning is a new AI approach that allows multiple hospitals to train AI models without sharing raw patient data. Link
- AI models will be trained on distributed datasets across different hospitals without exposing private data.
- This will significantly improve AI accuracy while maintaining patient confidentiality.
Real-World Implementation:
- Google’s AI division is pioneering federated learning for healthcare applications to ensure AI cancer detection models learn from global datasets while maintaining privacy.
- Mayo Clinic and NVIDIA are collaborating on federated AI models to improve medical imaging analysis for cancer detection. Link1, Link2
8. AI in Post-Treatment Cancer Monitoring
Artificial Intelligence (AI) won’t just stop at detection and treatment – it will also play a major role in post-treatment monitoring and recurrence prediction.
- AI will analyze follow-up scans to detect signs of cancer recurrence earlier than traditional methods.
- Wearable biosensors will use AI to monitor a patient’s vital signs and biochemical markers for early relapse detection.
Real-World Implementation:
- AI-powered MRI follow-up scans at Massachusetts General Hospital are detecting cancer recurrence months before traditional screenings. Link
- AI models at MD Anderson Cancer Center are analyzing follow-up data to predict recurrence risk based on post-treatment health metrics. Link
Conclusion
AI is revolutionizing cancer detection, offering higher accuracy, faster diagnosis, and personalized treatment options. While challenges such as data bias, regulatory hurdles, and clinical integration remain, ongoing advancements will drive AI adoption in healthcare. In the future, AI will not only assist doctors but also empower patients with real-time cancer detection tools, leading to better health outcomes worldwide.





