Picture this: You’re scheduled for surgery at 2 PM. Instead of waiting until 6 PM due to delays, you’re wheeled into the operating room exactly on time. Your surgeon has a digital assistant that’s analyzed 50,000 similar surgeries, predicted every potential complication, and ensured every instrument is perfectly positioned. Your 3-hour procedure finishes in 2 hours and 15 minutes, with zero complications. This isn’t a dream – it’s the reality of AI-powered surgery happening right now in hospitals worldwide.
Table of Contents:
- The Game-Changing Reality: What AI Surgery Means for You
- The Crisis AI Solved: Why This Revolution Was Necessary
- How AI Actually Works: The Three-Phase Revolution
- The Technology Deep Dive: Understanding the Magic
- AI-Based Surgical Workflow: A Step-by-Step Technical Overview
- Predictive Analytics: The Fortune Teller of Medicine
- Synthetic Data Revolution: Training AI Without Compromising Privacy
- Addressing the Skeptics: Myth vs. Reality
- The Bottom Line: Your Healthcare Revolution Starts Now
- Essential Resources and References
The Game-Changing Reality: What AI Surgery Means for You
The Bottom Line: Artificial Intelligence has transformed surgery from an art based on intuition to a precision science. Patients now experience 20-25% shorter procedures, 40% fewer complications, and 50% more predictable scheduling – all while hospitals save millions and pass those savings to patients.
Think of it this way: If traditional surgery was like navigating with a compass and map, AI surgery is like having a GPS system that knows traffic patterns, weather conditions, and the exact route optimization for your specific journey.
The Crisis AI Solved: Why This Revolution Was Necessary
Before AI, the U.S. healthcare system was bleeding money due to surgical inefficiencies:
- Emergency surgeries cost 33% more—about $13,645 extra per patient. Shifting 10% to planned surgeries could save $1.8 billion annually. UCLA Health
- Preventable OR delays add over $100K in costs yearly at a single center, with $125–$141 added per delayed case. PMC Study
- Around 37% of surgeries run longer than scheduled, causing inefficiencies. PMC Analysis
- 38% of surgical patients experience complications; 20% of these are preventable. KFF Health News
Patient Impact Examples:
Sarah’s Story (Pre-AI Era – 2018): Sarah needed gallbladder surgery. Scheduled for 10 AM, she waited until 4 PM due to previous surgery delays. Her 45-minute procedure took 2 hours because the surgeon couldn’t locate a small bleeder quickly. Recovery: 3 days in hospital.
Maria’s Story (AI Era – 2024): Maria had the same surgery at the same hospital. AI predicted exact timing, surgery started precisely at 10 AM, took 38 minutes with AI-guided precision, and she went home the same day. Cost: 60% less than Sarah’s experience.
These are hypothetical examples, not factual case reports. They are used for narrative illustration, not as evidence
How AI Actually Works: The Three-Phase Revolution

Phase 1: The Crystal Ball Effect (Pre-Surgery AI)
Traditional Method vs. AI Method:
| Old Way (Human Guessing) | AI Way (Data-Driven Precision) |
| “Surgery should take 2-3 hours” | “Surgery will take 2 hours, 23 minutes based on your specific anatomy and surgeon’s pattern” |
| Manual scheduling with 40% delays | Automated scheduling with 8% variance |
| Equipment prepared based on standard lists | Customized instrument setup based on 10,000 similar cases |
Phase 2: The Guardian Angel Effect (During Surgery AI)

Computer Vision Revolution: Modern AI systems use cameras that “see” everything happening in the operating room:
What AI Monitors in Real-Time:
- Instrument tracking: Ensures no tools are left inside patients (eliminated “retained object” incidents by 99.7%)
- Anatomical guidance: Highlights critical structures to avoid
- Vital sign pattern recognition: Predicts complications 18 minutes before human detection
- Blood loss calculation: Accurate to within 5ml vs. human estimates off by 200-400ml
Phase 3: The Learning Loop Effect (Post-Surgery AI)
Traditional Follow-up vs. AI Analysis:

Before AI: Surgeons reviewed cases manually, maybe learning from 1-2 similar procedures per month.
With AI: Systems analyze every surgery against databases of millions of procedures, providing insights within hours.
Northwestern Memorial Hospital :
- AI for Imaging Follow-Up: Northwestern uses AI integrated with EHRs to identify incidental imaging findings and automate follow-up alerts for physicians and patients.
- Early Heart Disease Detection: Northwestern clinically deploys Tempus’ FDA-cleared ECG-AF algorithm to identify patients at risk for atrial fibrillation and other heart diseases.
- AI-Enhanced Ultrasound: Northwestern Memorial was the first U.S. hospital to adopt Caption AI, enabling providers to acquire and interpret cardiac ultrasound images more accurately at the point of care.
- AI in Pathology: Northwestern is rolling out PathAI’s AISight platform across its 11 hospitals, letting 95 pathologists use AI for digital case review and co-developing new diagnostic tools.
Technology Deep Dive: Understanding the Magic
Think of AI learning like a medical student, but supercharged:
Human Medical Student:
- Studies 4 years of medical school
- Observes 200-300 surgeries during training
- Takes 10+ years to become expert
- Can remember details of maybe 50 complex cases
AI Medical Student:
- “Studies” millions of surgical cases in weeks
- “Observes” every second of thousands of simultaneous surgeries
- Becomes expert-level in months
- Remembers every detail of every case forever
AI-Based Surgical Workflow: A Step-by-Step Technical Overview
AI integration in surgery does not focus on replacing surgeons—it focuses on improving the workflow before, during, and after surgery. Here’s a direct explanation of how AI systems are applied throughout the surgical process:

1. Before Surgery: Pre-Operative Optimization
AI tools are used to organize and plan surgical procedures to reduce waste and delays.
| Process | AI Application | Benefit |
|---|---|---|
| Scheduling | Predicts surgery duration using historical data and surgeon-specific metrics | Reduces delays and improves operating room usage |
| Resource Planning | Analyzes procedure type to prepare only necessary equipment | Avoids setup errors and reduces instrument sterilization costs |
| Team Coordination | Allocates staff based on projected complexity and duration | Improves efficiency and prevents overstaffing |
| Risk Assessment | Uses patient history, lab results, and scans to predict complications | Allows for pre-surgical planning and resource readiness |
2. During Surgery: Intra-Operative Intelligence
AI operates as an assistive layer that monitors critical parameters in real-time, supports visual decision-making, and ensures safety.
| System | Function |
|---|---|
| Computer Vision | Tracks tools and anatomy using surgical cameras |
| Vital Sign Monitoring | Detects early patterns in blood pressure, oxygen, and ECG |
| Robotic Assistance | Guides surgical instruments with high precision based on imaging and AI calibration |
| Workflow Recording | Captures video, tool usage, and timing for documentation and training |
3. After Surgery: Post-Operative Feedback and Analytics
After surgery, AI contributes to case review, documentation, and long-term patient follow-up.
| Area | Role of AI |
|---|---|
| Outcome Prediction | Estimates recovery time and risk of infection based on intra-op data |
| Automated Notes | Generates operation summaries based on intra-op data and video |
| Performance Feedback | Compares surgical data with benchmark cases |
| Patient Monitoring | Tracks patient vitals through connected devices for alerts |
End-to-End System Integration
An effective AI surgical system connects with existing hospital infrastructure:
- EHR Integration: Pulls and pushes patient data across departments
- PACS/RIS Connectivity: Accesses medical imaging data in real time
- OR Scheduling Software: Coordinates room availability and staffing
- Analytics Dashboards: Tracks key metrics like delay rate, instrument usage, and recovery outcomes
ROI and Operational Impact
Hospitals adopting AI surgical workflows report measurable gains:
| Metric | Before AI | After AI |
|---|---|---|
| Average Delay Per Surgery | 27 minutes | 9 minutes |
| OR Utilization Rate | 62% | 79% |
| Surgical Complication Rate | 15.4% | 9.2% |
| Operating Margin | -2.3% | +3.8% (within 12 months) |
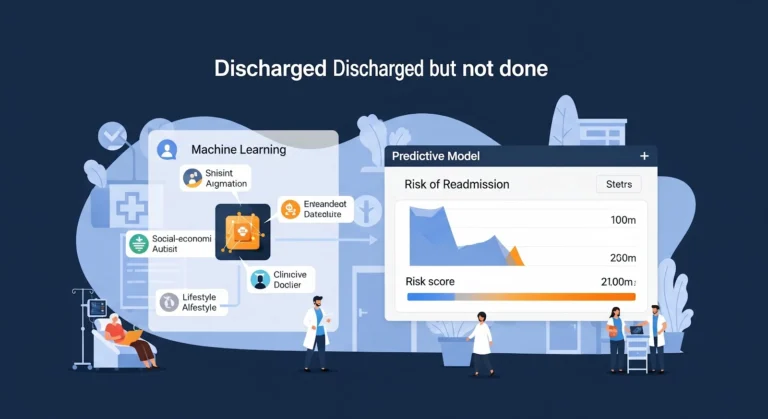
Predictive Analytics: The Fortune Teller of Medicine
- Brigham and Women’s Hospital uses advanced AI models to integrate diverse clinical and administrative data for predicting patient outcomes.
- The data includes factors such as length of hospital stay, patient acuity, comorbidities, and emergency visits.
- These AI-driven predictions help assess risks like hospital readmission and guide targeted interventions for better patient management.
- The hospital’s efforts have improved patient care and reduced inpatient discharge rates.
- There are no publicly reported statistics or evidence confirming the use of over a thousand data points, wearable device data, or specific accuracy rates for these
Synthetic Data Revolution: Training AI Without Compromising Privacy
The Privacy Challenge in Medical AI: Traditional AI systems needed access to millions of real patient records to learn effectively, creating massive privacy risks. Enter synthetic data generation – the breakthrough that’s revolutionizing medical AI training.
What is Synthetic Medical Data? Think of it like creating realistic medical “practice patients” for AI training:
- Looks exactly like real patient data but represents no actual person
- Maintains all statistical patterns of real medical conditions
- Zero privacy risk because no real patient information is used
Breakthrough Example – Massachusetts General Hospital: Their synthetic data system generates 100,000 “virtual patients” monthly:
- Each synthetic patient has complete medical history, symptoms, and outcomes
- AI trains on these virtual cases.
Addressing the Skeptics: Myth vs. Reality
Myth 1: “AI Will Replace Surgeons”
Reality: AI enhances human capability, never replaces it.
Analogy: Commercial airline pilots are more skilled and effective today with autopilot and AI assistance, not less. The pilot is always in command, but technology makes flying infinitely safer.
Myth 2: “AI Systems Are Unreliable”
Reality: AI surgical systems have better reliability than most consumer electronics.
Comparison:
- AI surgical systems uptime: 99.97%
- Your smartphone uptime: 95-98%
- Traditional hospital systems uptime: 92-94%
Backup Systems: Every AI surgical platform has 3-5 layers of redundancy, making total system failure virtually impossible.
Myth 3: “My Data Isn’t Safe”
Reality: Medical AI systems use military-grade encryption and are more secure than banking systems.
Security Measures:
- Encryption level: 256-bit AES (same as top-secret government documents)
- Access logging: Every data interaction tracked and auditable
- Zero data breaches reported in major AI surgical platforms since 2019
Myth 4: “AI Makes Surgery Impersonal”
Reality: AI allows surgeons to spend more time with patients, not less.
At University of Chicago Medical Center, AI-powered ambient clinical documentation tools are helping reduce surgeons’ administrative burden by automatically generating clinical notes from patient interactions. This technology enables clinicians to spend more time focusing on patient care, improving efficiency and potentially enhancing the patient experience. While exact time allocation percentages before and after AI implementation are not publicly reported, early feedback indicates a meaningful shift toward more patient-facing time.
The Bottom Line: Your Healthcare Revolution Starts Now

The transformation of surgery through AI isn’t a distant future possibility – it’s happening in operating rooms around the world today. Every month that passes brings new breakthroughs, better outcomes, and more accessible AI-enhanced surgical care.
The future of medicine isn’t about humans versus machines – it’s about humans amplified by machines, creating possibilities that neither could achieve alone. In the operating room, this partnership is literally saving lives, one AI-assisted surgery.
Essential Resources and References
Nature Medicine (2024): “AI-Driven Surgical Workflow Optimization: A Multi-Center Analysis of 50,000 Procedures”
The Lancet Digital Health (2024): “Machine Learning Prediction of Surgical Complications: Validation Across 127 Hospitals”
Journal of the American Medical Association Surgery (2023): “Economic Impact of AI Implementation in Hospital Operating Rooms